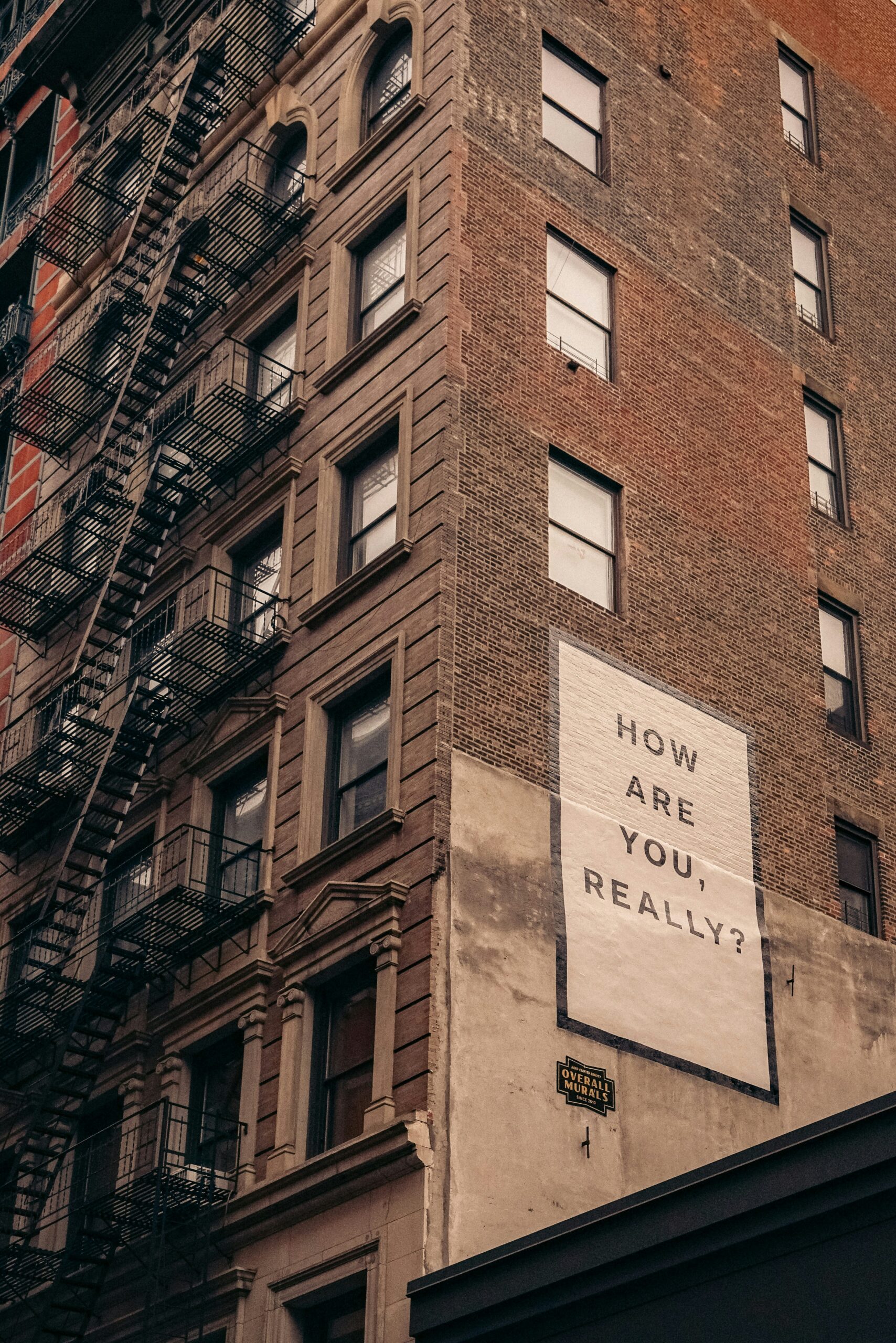
Depression is often thought of as a mental or emotional issue, but its effects go far beyond mood. It takes a serious toll on the body as well, influencing everything from immune function to heart health.
Many people struggling with depression experience physical symptoms they don’t immediately connect to their mental state. In this article, we’ll explore how depression impacts the body and why it’s crucial to address both mind and body in treatment:
- The physical symptoms of depression
- The impact on the nervous system
- Long-term health risks of depression
- Recognising physical symptoms can be key
The physical symptoms of depression
Depression can manifest in various physical ways, including chronic fatigue, muscle aches, digestive issues, and even unexplained pain. The brain and body are deeply connected, and when mental health suffers, so does physical health.
Let’s take a closer look at physical reactions to depression stressors:
Chronic fatigue and low energy: Many people with depression experience persistent tiredness, even after sleeping enough. Everyday tasks can feel exhausting due to disruptions in brain chemistry and sleep patterns.
Sleep disturbances: Depression is linked to insomnia (trouble falling or staying asleep) or hypersomnia (sleeping too much). Poor sleep quality can further worsen mood, cognitive function, and immune response.
Chronic pain and muscle aches: People with depression often report headaches, back pain, and muscle tension. This happens because depression affects neurotransmitters like serotonin and dopamine, which regulate pain perception.
Weakened immune system: Chronic stress and depression suppress the immune system, making individuals more prone to infections and illnesses. Increased inflammation in the body due to depression has been linked to conditions like heart disease and diabetes.
Digestive issues (gut-brain connection): Depression is associated with stomach pain, bloating, nausea, diarrhoea, or constipation. The gut microbiome plays a crucial role in mental health, and an imbalance can contribute to both depression and digestive problems.
Weight changes and appetite fluctuations: Some people experience weight gain due to emotional eating, while others lose weight due to a lack of appetite. This is influenced by disruptions in hunger-regulating hormones like ghrelin and leptin.
Cardiovascular risks: Depression increases the risk of high blood pressure, heart disease, and stroke. Chronic stress hormones like cortisol contribute to inflammation and damage blood vessels.
Cognitive decline and memory problems: Depression can cause brain fog, difficulty concentrating, and memory issues. Long-term depression is associated with a higher risk of neurodegenerative diseases like Alzheimer’s.
Hormonal imbalances: Depression affects the hypothalamic-pituitary-adrenal (HPA) axis, leading to disruptions in stress hormones like cortisol. This can contribute to irregular menstrual cycles, thyroid issues, and libido changes.
Increased sensitivity to pain: Studies show that people with depression are more sensitive to pain, even without an underlying medical condition.This is linked to reduced serotonin levels, which help regulate pain perception.
The impact on the nervous system
Depression affects the brain’s neurotransmitters, leading to imbalances in serotonin and dopamine, which regulate mood and pain perception. This is why many people with depression experience body aches and a lower tolerance for pain.
Neurotransmitters are chemical messengers that regulate mood, cognition, and bodily functions. Depression is associated with imbalances in several key neurotransmitters:
Serotonin (5-HT):
Often called the “feel-good” chemical, serotonin plays a crucial role in regulating mood, sleep, and appetite. In depression, serotonin levels are often lower, leading to increased feelings of sadness, fatigue, and anxiety.
Dopamine (DA):
The brain’s “reward” chemical, responsible for motivation and pleasure. Depression can reduce dopamine activity, leading to a lack of motivation, loss of interest in activities (anhedonia), and decreased pleasure from daily experiences.
Norepinephrine (NE):
Involved in the body’s stress response and alertness. Depression is linked to lower norepinephrine levels, contributing to fatigue, low energy, and difficulty concentrating.
“In people who are depressed, neuroscientists have noticed that the hippocampus in the brain—the region that helps regulate mood—is smaller.” – Harvard Health Publishing
Long-term health risks of depression
If left untreated, depression can contribute to long-term health risks such as heart disease, weakened immune function, and metabolic disorders. Chronic stress from depression leads to inflammation, which can trigger a host of physical illnesses.

Recognising physical symptoms can be key
Depression is more than just feeling sad: It’s a condition that affects the whole body. Recognising these physical symptoms is key to getting the right treatment:
- Chronic fatigue and low energy
- Sleep disturbances such as insomnia and hypersomnia
- Chronic pain and muscle aches
- Weakened immune system
- Digestive issues
- Weight changes and fluctuation in appetite
- Changes in blood pressure and heart health
- Brain fog and cognitive issues
- Hormonal imbalance
This page cannot replace a consultation with your GP. Please remember: Mental and physical health go hand in hand, and prioritising both is essential for overall well-being.